Platelet-Rich Plasma (PRP) and Its Role in Dental Surgery
2025-07-07 12:53:34
Platelet-Rich Plasma (PRP) and Its Role in Dental Surgery
Definition and Composition of PRP
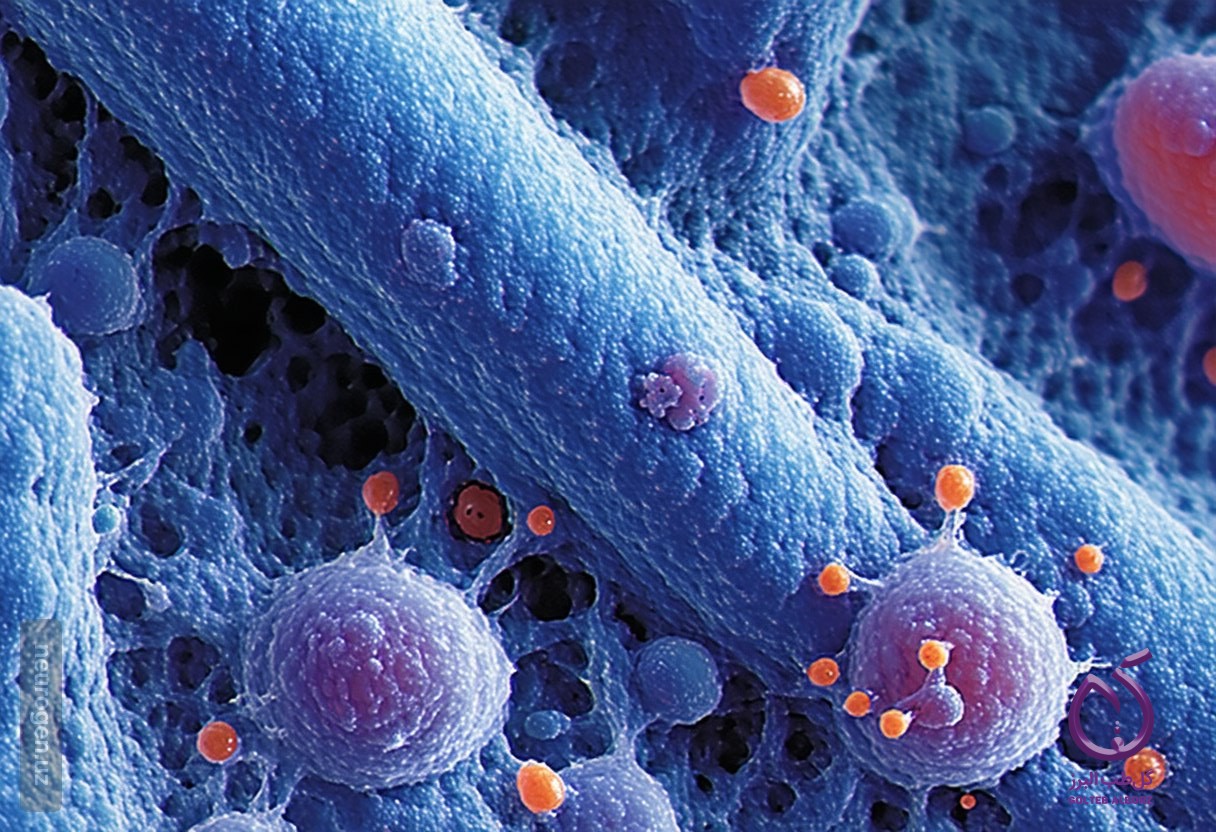
Platelet-rich plasma (PRP) is characterized by a high concentration of autologous platelets suspended in a small volume of autologous plasma. Specifically, PRP contains at least 1,000,000 platelets per microliter in a 5 mL volume, while normal platelet counts in human blood typically range from 150,000 to 350,000 platelets per microliter. Upon triggering coagulation at the wound site, the platelets release alpha granules that contain a variety of growth factors essential for tissue repair and osteogenesis. These growth factors play crucial roles in promoting cell proliferation, chemotaxis, and differentiation, thereby enhancing wound healing, accelerating bone repair, stimulating fibroblast proliferation, and increasing vascularity in tissues.
Key Growth Factors in PRP
The primary effects of PRP are largely attributed to platelet-derived growth factor (PDGF), which is vital for both hard and soft tissue healing. PDGF promotes chemotaxis, mitogenesis, and the replication of stem cells at injury sites, leading to matrix bone formation and angiogenesis through elevated levels of vascular endothelial growth factor (VEGF). This process can expedite soft tissue healing via neo-vascularization. Additionally, PDGF stimulates the production of fibronectin—a critical cell adhesion molecule—and hyaluronic acid, both of which facilitate cellular proliferation and migration during the healing process, including osteoconduction.
Application of PRP in Dental Surgery
In dental surgery, particularly following tooth extractions, PRP has emerged as a potential therapeutic strategy to enhance healing outcomes. Tooth extractions can often lead to significant postoperative pain and complications such as prolonged bleeding, especially in patients on anticoagulant therapy. Various techniques have been employed to mitigate these issues and promote healing, including the use of fibrin sponges and biostimulation with LASER.
Recent studies have explored the application of PRP to increase the concentration of growth factors that aid tissue regeneration. While some pilot studies have shown promising results—demonstrating improved soft tissue healing in patients treated with PRP compared to control groups—evidence supporting its efficacy in enhancing bone regeneration remains limited and somewhat controversial.
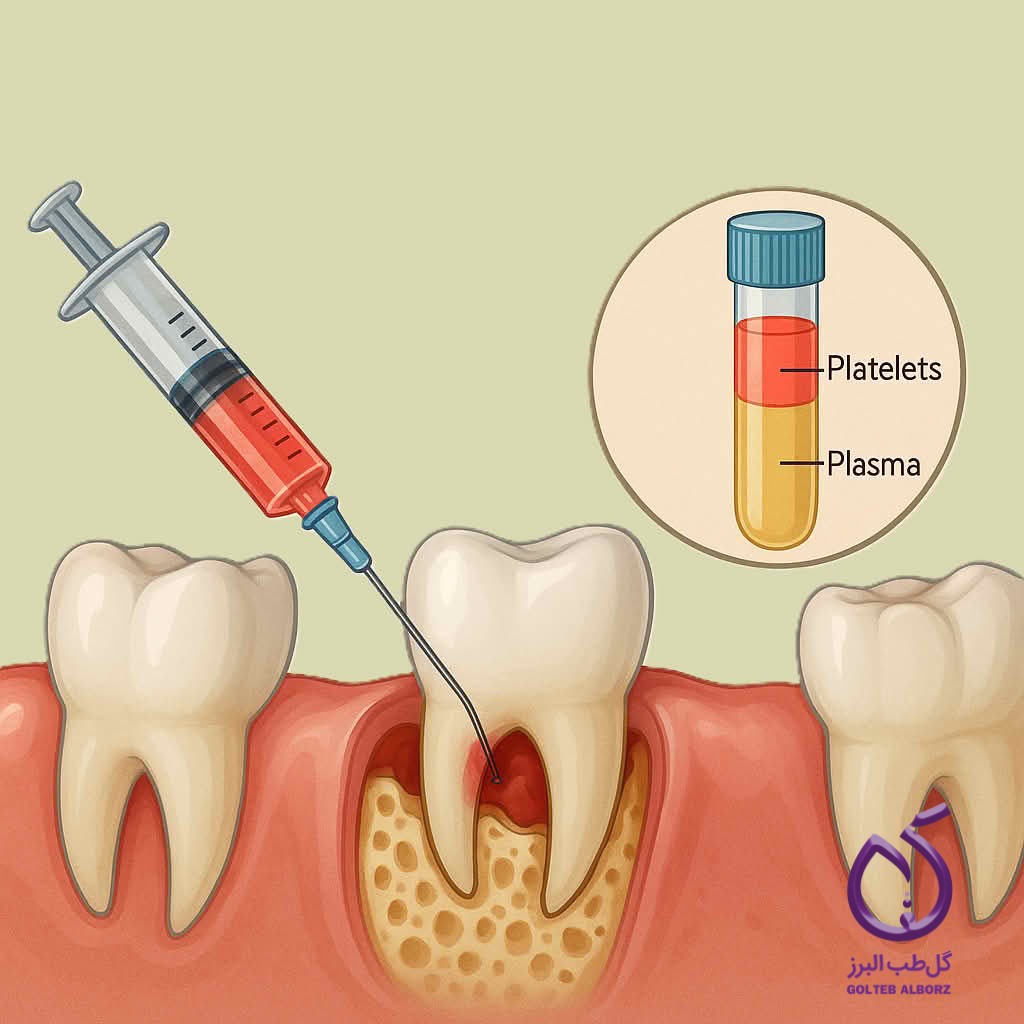
In one notable study, patients receiving PRP exhibited significantly improved soft tissue healing compared to those who did not receive treatment. Control group patients reported higher incidences of complications such as dry sockets and acute inflammation. Radiographic evaluations indicated significant differences in bone density patterns only for certain socket types. Furthermore, assessments of postoperative pain revealed that control group patients experienced significantly more pain during the initial days following extraction.
Conclusion
The literature suggests that while PRP can enhance soft tissue healing following tooth extractions, its effectiveness in promoting bone regeneration is less conclusive. The use of PRP appears to positively influence the early phases of bone healing, facilitating initial bone formation but showing diminishing effects after a few days. Further research is necessary to establish definitive conclusions regarding the long-term benefits and mechanisms of PRP in dental applications.
subscribe to newsletter
Find out about our latest discounts and news
Latest Articles
15
September
Get to Know the Endomotor Endowiseplus and Learn How to Use It
Read more
09
September
Practical training on the use of OraAid adhesives on a dental model
Read more
04
September
Do you know the role of silicone stops in endodontic treatments?
Read more
04
September
Tooth Discoloration After Root Canal | Causes and Treatment Options
Read more





